When we hear the word “trauma,” we often think of sadness, tears, and emotional wounds. But what if the impact of trauma runs much deeper than we imagined—what if it’s physically reshaping the brain of a child? That’s not fear-mongering. It’s neuroscience. Childhood trauma doesn’t just hurt feelings—it changes how the brain develops, how it processes information, and how it sees the world.
The Silent Architect: How Trauma Shapes the Developing Brain
During childhood, the brain is incredibly plastic. It adapts and rewires based on experiences. This is a good thing when children grow up in a loving, secure environment. But when exposed to repeated stress—like abuse, neglect, domestic conflict, or even chronic fear—the brain begins to mold itself for survival, not growth.
Researchers at Harvard’s Center on the Developing Child have found that persistent stress leads to toxic stress responses. These aren’t the normal ups and downs of childhood. Toxic stress disrupts the development of brain architecture and increases the likelihood of problems in learning, behavior, and health later in life.
Trauma Leaves Fingerprints on the Brain
Let’s break it down further. What physically happens in the brain?
- Amygdala (the brain’s fear center) becomes hyperactive. It’s always on alert. That’s why traumatized children often seem “jumpy” or overly anxious.
- Hippocampus (memory and emotion processor) can shrink. This affects how kids remember, learn, and regulate emotions.
- Prefrontal cortex (decision-making and self-control) development can be delayed. This explains the impulsivity and poor concentration seen in many trauma-affected kids.
In simpler terms, trauma puts a child’s brain into “survival mode.” Instead of learning, exploring, or playing, the brain is focused on staying safe.
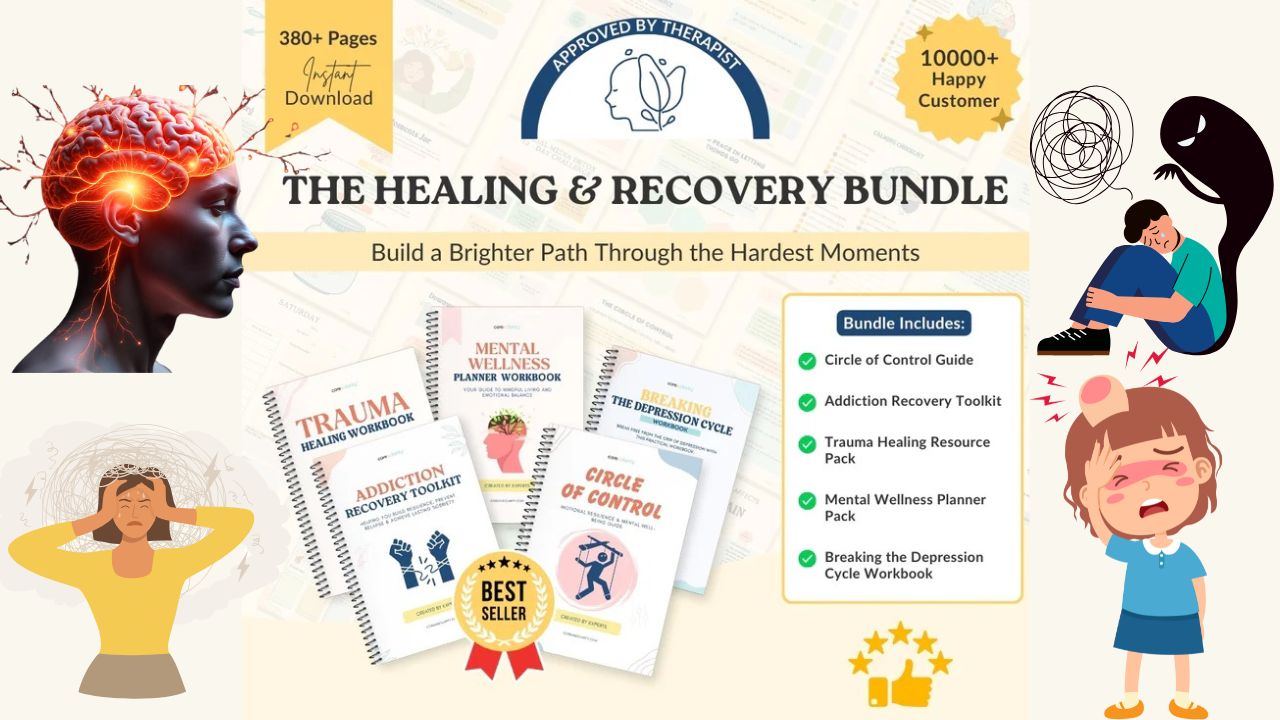
Get Your Trauma Recovery Bundle Now
It’s Not Just Mental—It’s Biological
You may notice a child overreacting to small frustrations. Or freezing in social situations. Or forgetting things they just learned. These aren’t character flaws or misbehavior. These are symptoms of a nervous system that’s been rewired to expect danger—even when there is none.
A study by the CDC and Kaiser Permanente known as the ACEs (Adverse Childhood Experiences) Study found that children with high trauma exposure have dramatically higher risks of:
- Learning difficulties
- Substance abuse
- Depression and anxiety
- Chronic diseases
- Suicidal thoughts
Early trauma affects not only the mind but also the immune system, hormone regulation, and long-term physical health.
The Hidden Faces of Trauma
Here’s what many parents don’t realize: trauma isn’t always one big event. It’s often a buildup of small, chronic stressors. These can include:
- Being constantly criticized
- Emotional unavailability of parents
- Moving homes frequently
- Witnessing adult conflict or divorce
- Living in poverty or community violence
Even kids who appear “fine” on the outside may carry invisible wounds.
A quiet child who always follows rules may be dissociating. A child who acts out constantly might not be seeking attention—they may be screaming for safety.
Why Understanding Trauma Matters
When we recognize trauma as a brain injury—not just a behavior issue—we shift how we respond. Instead of asking, “What’s wrong with this child?” we ask, “What happened to this child?”
This one change in perspective can make all the difference.
Rather than punishment, these children need patience.
Rather than lectures, they need connection.
Rather than fixing them, they need healing.
And healing begins when we stop blaming them for the scars they didn’t choose.
What Doctors and Therapists Are Saying
Dr. Bruce Perry, a leading child trauma psychiatrist, says:
“The more healthy relationships a child has, the more likely he will be to recover from trauma and thrive. Relationships are the agents of change.”
That means your presence, your calm voice, your patience—it all matters more than any therapy session.
Dr. Bessel van der Kolk, author of The Body Keeps the Score, explains:
“Traumatized people chronically feel unsafe inside their bodies… Trauma compromises the brain area that communicates physical, embodied feeling and the sense of being alive.”
This is why children often struggle to articulate what they feel. Their trauma lives in the body before it can be translated into words.
Practical Steps to Support a Traumatized Child
- Create a safe, predictable environment
Routines reduce anxiety. Calm tones and consistent boundaries help children feel secure. - Regulate before you educate
When a child is triggered, they can’t think logically. Help them feel safe first—then teach or guide. - Model emotional regulation
Your calm presence can co-regulate a child’s overwhelmed nervous system. - Validate feelings without judgment
“You’re safe now.” “That was really scary, wasn’t it?” These phrases reassure and build trust. - Use trauma-informed tools
Workbooks, breathing exercises, and sensory-based grounding techniques give children coping mechanisms.
Final Words: The Hope Within the Hurt
If trauma can change the brain, then safety, connection, and love can heal it.
Brains are not broken. They are protective. What once helped a child survive can, with support, be reshaped to help them thrive. Neuroplasticity means healing is always possible.
Whether you’re a parent, teacher, or caregiver, your response to a child’s pain matters more than you know. The science is clear, but so is the heart of the matter:
No child is too far gone. No brain is too damaged. No story is too late to rewrite.
Let’s stop seeing trauma as invisible. Let’s start seeing it as a call to understand, to connect, and to heal—one child, one safe space, one loving moment at a time.
What counts as childhood trauma?
Any event or ongoing situation that overwhelms a child’s ability to cope, such as abuse, neglect, witnessing violence, or significant loss. Even seemingly “normal” events like bullying can be traumatic depending on the child’s sensitivity.
How does trauma affect a child’s brain differently than an adult’s?
Children’s brains are still developing, so trauma disrupts critical growth phases, altering neural connections. Adults have more stable brain structures, so while trauma impacts them, it’s less likely to fundamentally reshape their brain’s architecture.
Can a child fully recover from trauma’s brain effects?
Yes, with early intervention, safe environments, and therapies, neuroplasticity allows the brain healing. However, recovery varies based on trauma severity and timing.
How can I tell if my child’s behavior is from trauma or something else?
Look for persistent changes in mood, behavior, or physical health after a stressful event. Consult a pediatrician or therapist for assessments to distinguish trauma from conditions like ADHD or anxiety.
Also Read : Why Your Child’s Brain is Shrinking in this Modern Era